Gluteal Tendinopathy - What To Do When Physical Therapy Doesn’t Work
What Is The Anatomy And Function Of The Gluteal Muscles And Tendons?
The gluteus medius and gluteus minimus muscles are located on the side of the hip. The muscles originate on the top part of the hip and insert onto the lateral (outside) part of the femur (thigh bone) at a location called the greater trochanter.
Gluteus medius and gluteus minimus anatomy. Image is courtesy of Royal Orthopaedic Hospital.
The function of the gluteus medius and gluteus minimus muscles and tendons is to abduct the thigh (move the thigh straight to the side and up). The muscles also prevent the pelvis from dropping when walking or running.
An action of the gluteus medius muscle is hip abduction. Image is courtesy of Royal Orthopaedic Hospital.
An action of the gluteus medius muscle is to keep the pelvis from dropping on one side when walking or running. Image is courtesy of Royal Orthopaedic Hospital.
What Is Gluteal Tendinopathy?
Gluteal tendinopathy is a chronic degenerative change of the tendons on the lateral (outside) part of the hip caused by a repetitive cycle of microtrauma and improper healing (Bhabra et al., Orthop J Sports Med, 2016). It is important to note that while culturally the condition is often termed hip bursitis or hip tendinitis, it is not actually a condition of inflammation.
What Are The Symptoms Of Gluteal Tendinopathy?
Patients with gluteal tendinopathy typically present with the following symptoms:
Pain at the lateral (outside) part of the hip. The pain can spread down the outside part of the thigh.
Pain with laying or sleeping on the affected side.
Pain with activities such as stair climbing, squats, or lunges.
Pain when getting out of a chair.
Does Physical Therapy Usually Work?
Physical therapy is a first-line treatment for gluteal tendinopathy and provides significant benefit in most cases. However, previous studies show 10% to 40% of patients with gluteal tendinopathy do not improve with non-operative treatment (Walsh et al., J Arthroplasty, 2011).
What Are Treatment Options When Physical Therapy Does Not Work?
Corticosteroid (Cortisone) Injection
Corticosteroid injections are anti-inflammatory treatments that have been used for decades for various tendon conditions. Most studies show there is short term benefit of a few weeks to months, but the recurrence rate of symptoms is high (Rasmussen et al., Scand J Rheumatol, 1985; Rompe et al., Am J Sports Med, 2009; Shbeeb et al., J Rheumatol, 1996; Williams et al., Anesth Analg, 2009).
Recent studies show cortisone injections may be harmful to tendons. Specifically, a recent systematic review of 16 basic science studies showed cortisone may decrease tenocyte (tendon cell) viability and function while also weakening the structure of the tendon (Puzzitiello et al., Arthrosc Sport Med Rehabil, 2020).
Platelet-Rich Plasma (PRP) Injection
Given the frequent failure of physical therapy and cortisone injections, interest has emerged in the use of other treatment options such as platelet-rich plasma (PRP).
A recent landmark study evaluated the use of PRP for the treatment of gluteal tendinopathy (Fitzpatrick et al., Am J Sports Med, 2019). The purpose of the study was to determine if there would be sustained long-term differences in pain and function between patients receiving corticosteroid injection (CSI) and patients receiving PRP injection.
The study was a prospective randomized double-blind controlled trial of 80 patients divided into a CSI group and a PRP group. The groups were similar in composition. Patients had symptoms for at least 4 months prior to injection.
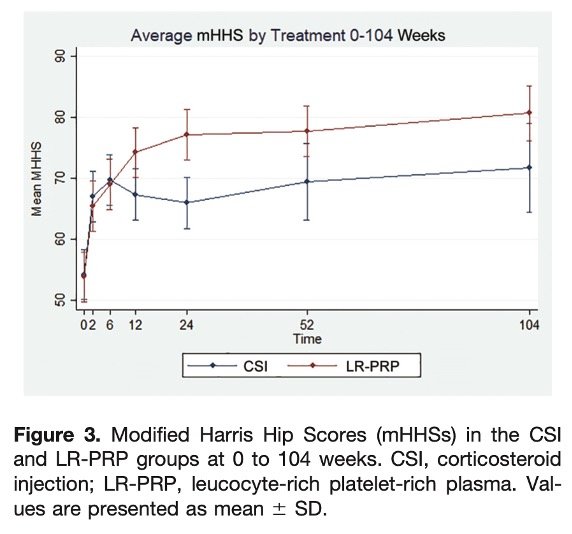
The study results showed the CSI group had maximal improvement at 6 weeks after injection, but the improvement was not maintained beyond 24 weeks after injection. In comparison, the PRP group had a greater improvement in pain and function compared to the CSI group, with improvement sustained at 2-year follow-up. Figure below illustrates the findings.
Graph showing patients receiving PRP injection for gluteal tendinopathy had better pain and function compared to patients receiving CSI over 2 year follow-up. Note: Higher mHHS scores indicate better levels of pain and function. (Fitzpatrick et al., Am J Sports Med, 2019)
Ultrasound-Guided Percutaneous Needle Tenotomy (Tenex)
Schematic of Tenex procedure (Baker et al., Orthop J Sports Med, 2020)
Another treatment option is ultrasound-guided percutaneous needle tenotomy (Tenex). A recent study evaluated pain and function outcomes in a case series of 29 patients with average follow-up of 22 months. All patients had symptoms for at least 4 months and failed conservative treatment prior to the procedure.
The study results showed pain and function scores significantly improved at the final follow-up and improvement overall was sustained. The majority of patients indicated they would have the procedure again (Baker et al., Orthop J Sports Med, 2020).
Take Home Points
Gluteal tendinopathy is a chronic degenerative change of the gluteal tendons which may result in pain at the side of the hip when:
Laying on one’s side (sleeping)
Going up and down stairs
Getting out of a chair or car
Doing squats or lunges
Physical therapy is a first-line treatment which has shown to be effective for most cases.
While cortisone may provide short-term benefit for pain relief, studies show the effect is short in duration and can actually be harmful the tendon.
PRP is an effective treatment showing durable sustained improvement in pain and function for patients who have not improved with physical therapy.
Ultrasound-guided percutaneous needle tenotomy is also an effective treatment showing durable sustained improvement in pain and function for patients who have not improved with physical therapy.
Appointment
Dr. Verma provides treatment for numerous orthopaedic and sports medicine conditions, including ultrasound-guided procedures such as PRP and Tenex for conditions like gluteal tendinopathy. If you are a patient interested in exploring treatment for your condition, please schedule a consultation with Dr. Verma to discuss the available options.
References
Royal Orthopaedic Hospital – Gluteal Tendinopathy. roh.nsh.uk. https://roh.nhs.uk/services-information/therapy/gluteal-tendinopathy
Bhabra G, Wang A, Ebert JR, Edwards P, Zheng M, Zheng MH. Lateral Elbow Tendinopathy: Development of a Pathophysiology-Based Treatment Algorithm. Orthop J Sports Med. 2016;4(11):2325967116670635. Published 2016 Nov 1. doi:10.1177/2325967116670635
Walsh MJ, Walton JR, Walsh NA. Surgical repair of the gluteal tendons: a report of 72 cases. J Arthroplasty. 2011;26(8):1514-1519.
Rasmussen Ege KJ, Fanø N. Trochanteric bursitis treatment by cor- ticosteroid injection. Scand J Rheumatol. 1985;14:417-420.
Rompe JD, Segal NA, Cacchio A, Furia JP, Morral A, Maffulli N. Home training, local corticosteroid injection, or radial shock wave therapy for greater trochanter pain syndrome. Am J Sports Med. 2009;37(10):1981-1990.
Shbeeb MI, O’Duffy JD, Michet CJ Jr, O’Fallon WM, Matteson EL. Evaluation of glucocorticosteroid injection for the treatment of tro- chanteric bursitis. J Rheumatol. 1996;23(12):2104-2106.
Williams BS, Cohen SP. Greater trochanteric pain syndrome: a review of anatomy, diagnosis and treatment. Anesth Analg. 2009;108(5):1662- 1670.
Puzzitiello RN, Patel BH, Forlenza EM, et al. Adverse Impact of Corticosteroids on Rotator Cuff Tendon Health and Repair: A Systematic Review of Basic Science Studies. Arthrosc Sports Med Rehabil. 2020;2(2):e161-e169. Published 2020 Apr 8. doi:10.1016/j.asmr.2020.01.002
Fitzpatrick J, Bulsara MK, O'Donnell J, Zheng MH. Leucocyte-Rich Platelet-Rich Plasma Treatment of Gluteus Medius and Minimus Tendinopathy: A Double-Blind Randomized Controlled Trial With 2-Year Follow-up. Am J Sports Med. 2019;47(5):1130-1137. doi:10.1177/0363546519826969
Baker CL Jr, Mahoney JR. Ultrasound-Guided Percutaneous Tenotomy for Gluteal Tendinopathy. Orthop J Sports Med. 2020;8(3):2325967120907868. Published 2020 Mar 19. doi:10.1177/2325967120907868