PRP and Tenex for Plantar Fasciitis — Treatment Options Beyond Rehabilitation and Shoe Modifications
What is the plantar fascia?
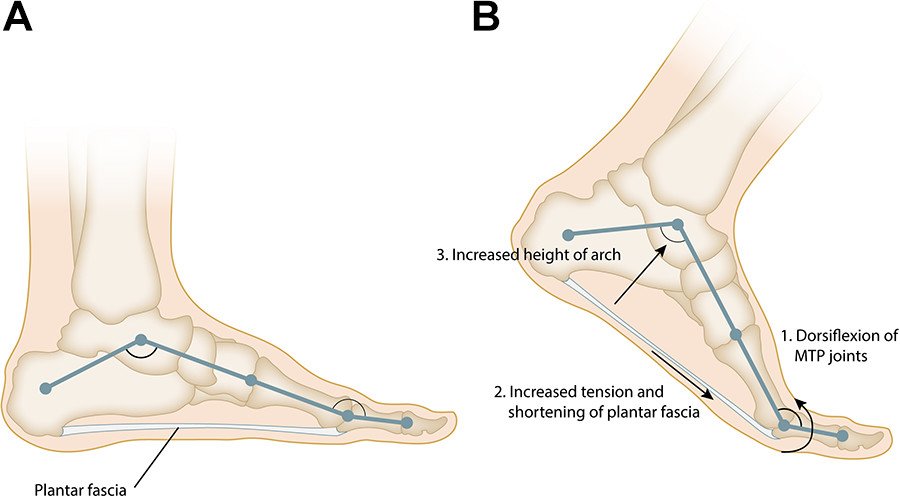
The plantar fascia is a band of tissue at the bottom of the foot that connects the heel bone (calcaneus) to the toes. The function of the plantar fascia is to support the arch of the foot and to also serve as a shock absorber when walking.
Figure 1 – Schematic photo showing plantar fascia and arch of foot. Image courtesy of Latt et al., Foot and Ankle Orthopaedics, 2020.
What is plantar fasciitis?
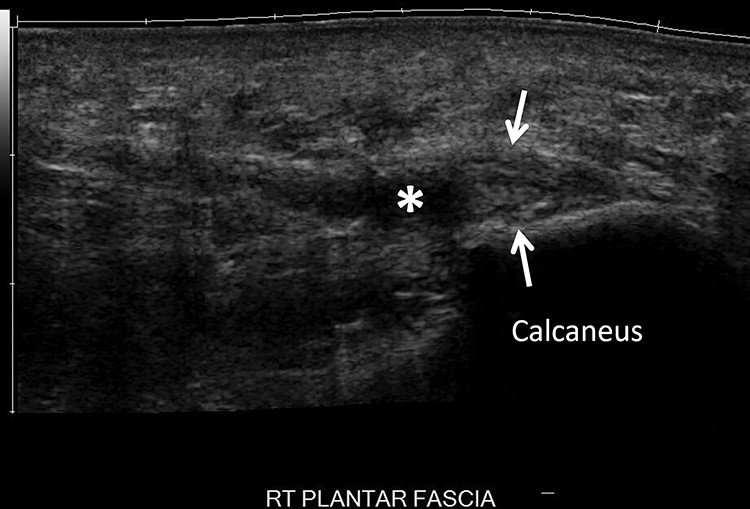
The term plantar fasciitis is somewhat of a misnomer, as the term “fasciitis” implies the presence of inflammation. In fact, once symptoms have been present for at least two weeks, there is little inflammation present. Instead, the plantar fascia fibers become disorganized, thickened and may even develop small partial tears. This wear pattern is more accurately termed “plantar fasciosis.”
Figure 2 - Diagnostic musculoskeletal ultrasound image of a thickened plantar fascia with partial tear. Arrows refer to increased thickness while asterisk corresponds to partial tear. Image courtesy of Latt et al., Foot and Ankle Orthopaedics, 2020.
What are the symptoms of plantar fasciitis?
Patient typically describe the following symptoms associated with plantar fasciitis:
Pain at the sole of the foot, particularly at the heel
Pain at the heel which is present when first getting out of bed in the morning, but somewhat improves with more walking.
Pain at the heel towards the middle and end of the day after walking or standing for long periods of time
What are treatment options for plantar fasciitis?
First-line management typically consists of evaluation of the arch of the foot and walking/running biomechanics. Often an arch support (orthotic) may be beneficial to reduce stress placed on the plantar fascia. Physical therapy may also be beneficial via stretching, strengthening, and manual or instrument-assisted treatments.
What if arch supports and physical therapy do not help?
Despite best efforts via physical therapy and arch supports, patients may still have symptoms traceable to plantar fasciitis. In this scenario, there are additional minimally invasive treatment options available.
Corticosteroid (Cortisone) Injections
Corticosteroid injections are anti-inflammatory treatments that have been used for decades for various tendon conditions and plantar fasciitis. The plantar fascia can be thought of as a tendon given as its normal structure and attachment to bone is similar.
Most studies show there is short term benefit of a few weeks to months, but the recurrence rate of symptoms is high (Rasmussen et al., Scand J Rheumatol, 1985; Rompe et al., Am J Sports Med, 2009; Shbeeb et al., J Rheumatol, 1996; Williams et al., Anesth Analg, 2009).
Recent studies show cortisone injections can be harmful to tendons. Specifically, a recent systematic review of 16 basic science studies showed cortisone may decrease tenocyte (tendon cell) viability and function while also weakening the structure of the tendon (Puzzitiello et al., Arthrosc Sport Med Rehabil, 2020).
Specifically pertaining to the plantar fascia, several potential complications of corticosteroid use exist, including plantar fascia rupture, skin atrophy, and fat pad atrophy. A previous study reported plantar fascia rupture was observed in 2.4% of patients who received corticosteroid injection for plantar fasciitis (Kim et al., Foot Ankle Spec, 2018)
Platelet-Rich Plasma (PRP)
Given the frequent failure of physical therapy and cortisone injections, interest has emerged in the use of other treatment options such as platelet-rich plasma (PRP).
A recent systematic review evaluated patient outcomes after PRP and corticosteroid injection (Hurley et al., Orthop J Sports Med, 2020). The study measured pain score (VAS) and American Orthopaedic Foot and Ankle Society (AOFAS) score, which evaluates patient pain and function. Scores were compared between the PRP and corticosteroid groups at 1, 1.5-, 3-, 6-, and 12-month time points.
9 randomized controlled trials were included in the study, encompassing 239 patients who underwent PRP injection and 240 patients who underwent corticosteroid injection.
The results showed the following:
Patients who underwent PRP injection had statistically significant better VAS pain scores than those who underwent corticosteroid injection at 1, 1.5-, 3-, 6-, and 12-month follow-up.
While there was no significant in difference in AOFAS scores at 1- and 3-month follow-up, patients who underwent PRP injection had statistically significant better AOFAS score at 6- and 12-month follow-up.
For patients with chronic pain due to plantar fasciitis, current clinical evidence suggests PRP may lead to greater short-term and long-term improvement in pain and function compared to corticosteroid injection.
Tenex (Ultrasound-Guided Percutaneous Needle Tenotomy)
Another treatment option is ultrasound-guided percutaneous needle tenotomy with Tenex.
A prospective case series of 12 patients with plantar fasciitis who had not improved with conservative care (physical therapy, orthotics, shockwave, corticosteroid injection) evaluated patient satisfaction, symptom resolution, and AOFAS scores at 3 and 24 months (Patel, American Journal of Orthopaedics, 2015).
The study results showed:
Resolution of pain in 11 of 12 patients by 3 months and sustained at 12-month follow-up
Improvement in AOFAS scores from mean of 30 (before procedure) to 88 (post-procedure).
Although the sample size is small, the study results suggest ultrasound-guided percutaneous needle tenotomy (Tenex) procedure may provide a long-term sustainable solution for plantar fasciitis.
Key Takeaways
Plantar fasciitis is a common cause of foot pain that can significantly reduce overall function and quality of life
Typical first-line treatments include physical therapy and orthotics
PRP and Tenex are minimally invasive evidence-based interventions which may provide a sustainable solution for plantar fasciitis when physical therapy and orthotics do not work
Appointment
Dr. Verma provides treatment for numerous orthopaedic and sports medicine conditions, including ultrasound-guided procedures such as PRP and Tenex for conditions like plantar fasciitis. If you are a patient interested in exploring treatment for your condition, please schedule a consultation with Dr. Verma to discuss the available options.
References
Latt LD, Jaffe DE, Tang Y, Taljanovic MS. Evaluation and Treatment of Chronic Plantar Fasciitis. Foot & Ankle Orthopaedics. 2020;5(1).
Rasmussen Ege KJ, Fanø N. Trochanteric bursitis treatment by corticosteroid injection. Scand J Rheumatol. 1985;14:417-420.
Rompe JD, Segal NA, Cacchio A, Furia JP, Morral A, Maffulli N. Home training, local corticosteroid injection, or radial shock wave therapy for greater trochanter pain syndrome. Am J Sports Med. 2009;37(10):1981-1990.
Shbeeb MI, O’Duffy JD, Michet CJ Jr, O’Fallon WM, Matteson EL. Evaluation of glucocorticosteroid injection for the treatment of trochanteric bursitis. J Rheumatol. 1996;23(12):2104-2106.
Williams BS, Cohen SP. Greater trochanteric pain syndrome: a review of anatomy, diagnosis and treatment. Anesth Analg. 2009;108(5):1662- 1670.
Puzzitiello RN, Patel BH, Forlenza EM, et al. Adverse Impact of Corticosteroids on Rotator Cuff Tendon Health and Repair: A Systematic Review of Basic Science Studies. Arthrosc Sports Med Rehabil. 2020;2(2):e161-e169. Published 2020 Apr 8. doi:
Kim C, Cashdollar MR, Mendicino RW, Catanzariti AR, Fuge L. Inci- dence of plantar fascia ruptures following corticosteroid injection. Foot Ankle Spec. 2010;3:335-337.
Hurley ET, Shimozono Y, Hannon CP, Smyth NA, Murawski CD, Kennedy JG. Platelet-Rich Plasma Versus Corticosteroids for Plantar Fasciitis: A Systematic Review of Randomized Controlled Trials. Orthop J Sports Med. 2020;8(4):2325967120915704. Published 2020 Apr 27.
Patel MM. A novel treatment for refractory plantar fasciitis. Am J Orthop (Belle Mead NJ). 2015;44(3):107-110.