Ultrasound-Guided Injections – A Review of the Evidence
Introduction
Musculoskeletal ultrasound involves the use of high-frequency sound waves to image soft tissue and bony surfaces. While musculoskeletal ultrasound has a strong base of evidence for use diagnostically , it is also used to perform injections and other procedures.
Injections are a common part of treatment plans in orthopaedics and sports medicine, providing therapeutic relief of pain and improvement in function. Furthermore, injections may be used as a diagnostic tool to guide treatment.
Injections were traditionally performed based upon feel, otherwise termed “palpation-guided” or “landmark-guided.” Over the past 10-15 years the application of musculoskeletal ultrasound has enabled the performance of ultrasound-guided injections.
The purpose of this blog post is to examine the evidence regarding ultrasound-guided injections to determine if and when they may be beneficial for patients.
Interventional Applications
Musculoskeletal ultrasound is used as tool to guide various types of procedures including the following:
Injections (therapeutic and diagnostic)
Aspiration (removing fluid from a swollen joint)
Tenotomy (poking a needle at damaged tendon tissue to promote healing)
Releases (common for carpal tunnel syndrome and trigger fingers)
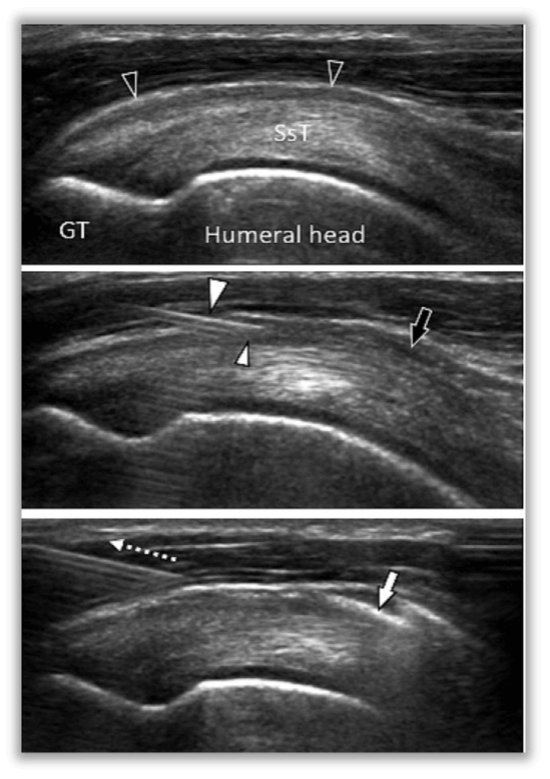
Figure 1 - Schematic of ultrasound-guided subacromial bursa injection for rotator cuff impingement (Molini et al., 2012)
Figure 2 - Visualization of needle during ultrasound-guided subacromial bursa injection for rotator cuff impingement (Molini et al., 2012)
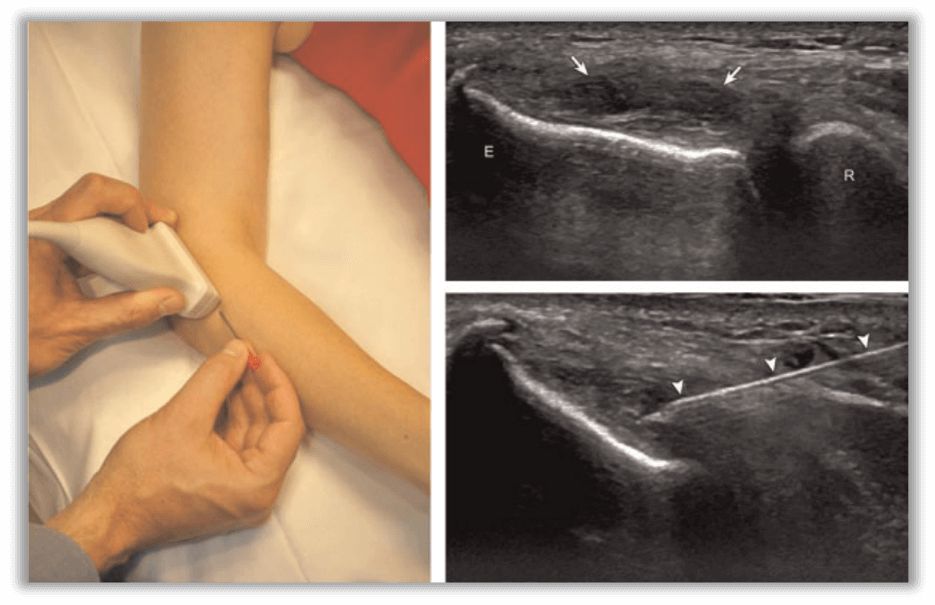
Figure 3 - Procedural set-up and ultrasound image of percutaneous needle tenotomy for elbow common extensor tendinosis (Tennis Elbow) (Chiavaras et al., 2013)
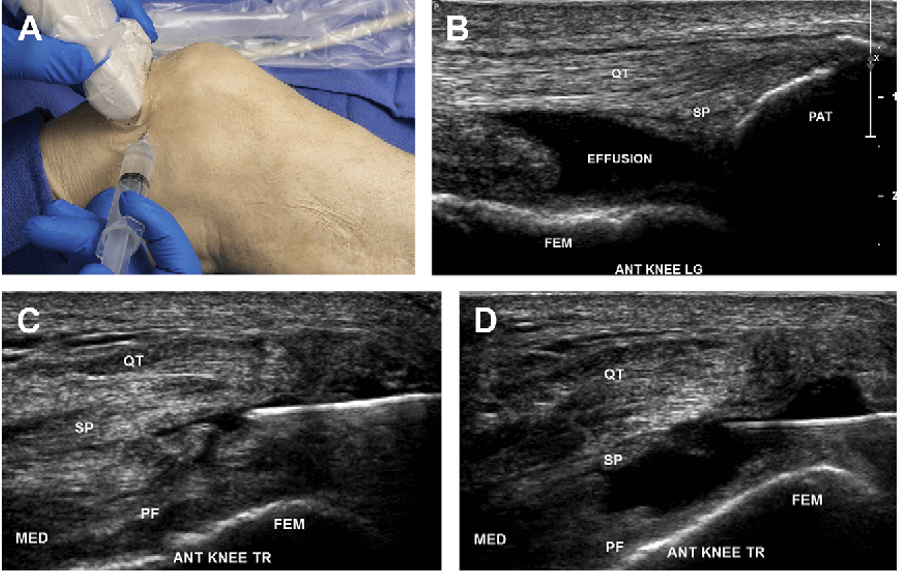
Figure 4 - Ultrasound-guided knee joint aspiration. QT = quadriceps tendon, SP = suprapatellar fat pad, FEM = femur, PF = pre-femoral fat pad, MED = medial, ANT = anterior, PAT = patella, TR = transverse, LG = long (Lueders et al, 2016).
Evidence Review
The efficacy and comfort associated with ultrasound-guided injections has been evaluated and compared with palpation-guided injections.
A 2015 systematic review and meta-analysis of 4 cadaveric studies (300 cadaveric shoulders) and 9 live human studies (514 patients) by Aly et al. evaluated ultrasound-guided and landmark-guided shoulder girdle injections. The results showed:
Ultrasound-guided glenohumeral joint injections and long head biceps brachii tendon sheath injections were significantly more accurate than landmark-guided injections.
There was no significant difference in accuracy for subacromial bursa injections.
There was significantly greater efficacy (improved pain and function at 6 weeks post-injection) in patients who received ultrasound-guided subacromial injection.
| USG | LMG | |
|---|---|---|
| Subacromial | 65% | 70% |
| LHBBT | 86.7% | 26.7% |
| Glenohumeral | 92.5% | 72.5% |
A 2011 randomized control trial by Sibbitt et al. evaluated 94 knees with osteoarthritis that were randomized to palpation-guided and ultrasound-guided corticosteroid injection. Outcomes evaluated included baseline pain, procedural pain, pain at outcome (2 weeks and 6 months), responders, therapeutic duration, reinjection rates, total cost, and cost per responder.
Relative to conventional palpation-guided anatomic landmark methods, ultrasound guidance for injection of the knee resulted in the following statistically significant findings:
48% reduction in procedural pain
42% reduction in pain scores at outcome
107% increase in responder rate
There was also a 13% reduction in cost per patient per year, and a 58% reduction in cost per responder per year.
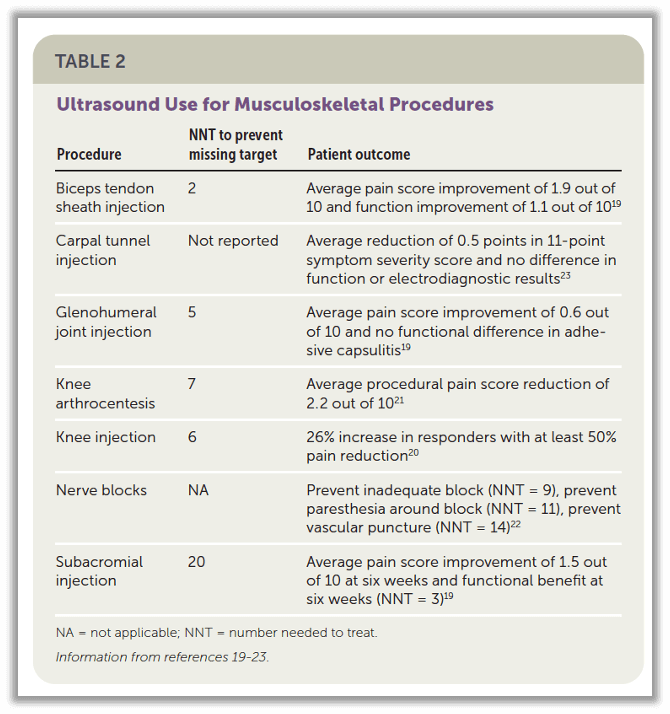
Furthermore, a 2020 review by Arnold et al. demonstrated ultrasound-guidance results in increased accuracy of injections compared to landmark- or palpation-guided injections for various injection types with a low NNT (number needed to treat to prevent missing the injection target) compared to landmark-guided injections.
Figure 6 - Data showing low NNT (number needed to treat) to prevent missing injection target for biceps tendon sheath, glenohumeral joint, knee joint aspiration, and knee joint injection (Arnold et al., 2020).
Patient Safety
Ultrasound can visualize blood vessels, nerves, and other structures of interest that may be in the pathway of a needle as it approaches the injection target. This allows the needle to be safely maneuvered around the aforementioned structures, resulting in improved patient safety.
Conclusions
The literature shows certain ultrasound-guided injections can improve clinical outcomes, reduce procedural pain, and improve cost-effectiveness compared to landmark- or palpation-guided injections.
– Rajiv Verma, DO RMSK
References
Molini L, Mariacher S, Bianchi S. US guided corticosteroid injection into the subacromial-subdeltoid bursa: Technique and approach. J Ultrasound. 2012;15(1):61-68.
Chiavaras MM, Jacobson JA. Ultrasound-guided tendon fenestration. Semin Musculoskelet Radiol. 2013;17(1):85-90.
Lueders DR, Smith J, Sellon JL. Ultrasound-Guided Knee Procedures. Phys Med Rehabil Clin N Am. 2016 Aug;27(3):631-48.
Aly AR, Rajasekaran S, Ashworth N. Ultrasound-guided shoulder girdle injections are more accurate and more effective than landmark-guided injections: a systematic review and meta-analysis. Br J Sports Med. 2015;49(16):1042-1049.
Sibbitt WL Jr, Band PA, Kettwich LG, Chavez-Chiang NR, Delea SL, Bankhurst AD. A randomized controlled trial evaluating the cost-effectiveness of sonographic guidance for intra-articular injection of the osteoarthritic knee. J Clin Rheumatol. 2011;17(8):409-415.
Arnold MJ, Jonas CE, Carter RE. Point-of-Care Ultrasonography. Am Fam Physician. 2020;101(5):275-285.